Search POM Topics
Iron Infusion
References
- Meta-analysis of the association between preoperative anaemia and mortality after surgery - BJS 2015
- Effects of restrictive red blood cell transfusion on the prognoses of adult patients undergoing cardiac surgery - a meta-analysis of randomized controlled trials - Critical Care 2018
- Restrictive or Liberal Red-Cell Transfusion for Cardiac Surgery - TRICS III - NEJM 2017
- A Multicentre, randomized, controlled clinical trial of transfusion requirements in Critical Care- TRICC - NEJM 1999
- Liberal transfusion strategy improves survival in perioperative but not in crtically ill patients - a meta-analysis of randomised trials - BJA 2015
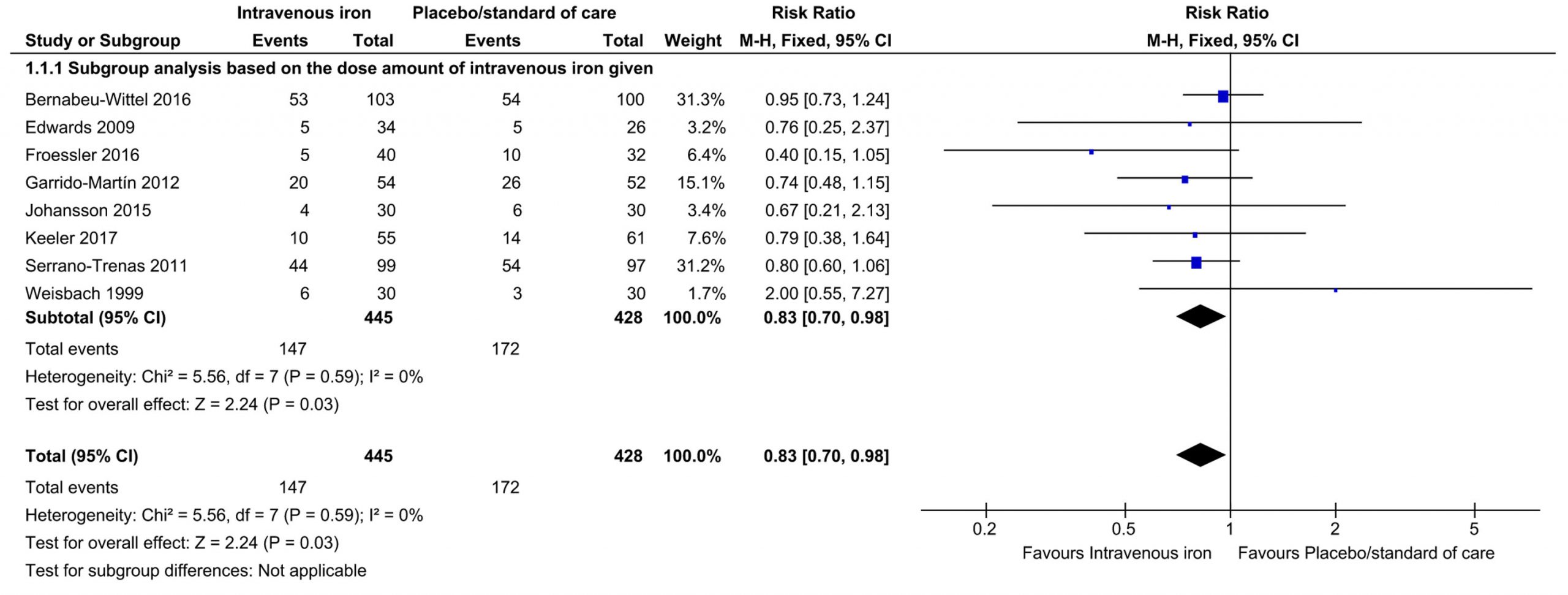
- Iron therapy for preoperative anaemia - Cochrane 2019
- The Important Role for Intravenous Iron in Perioperative Patient Blood Management in Major Abdominal Surgery - Annals of Surgery 2016
- Role or Preoperative IV Iron Therapy to Correct Anemia Before Major Surgery - Systematic Review and Meta-Analysis - 2021
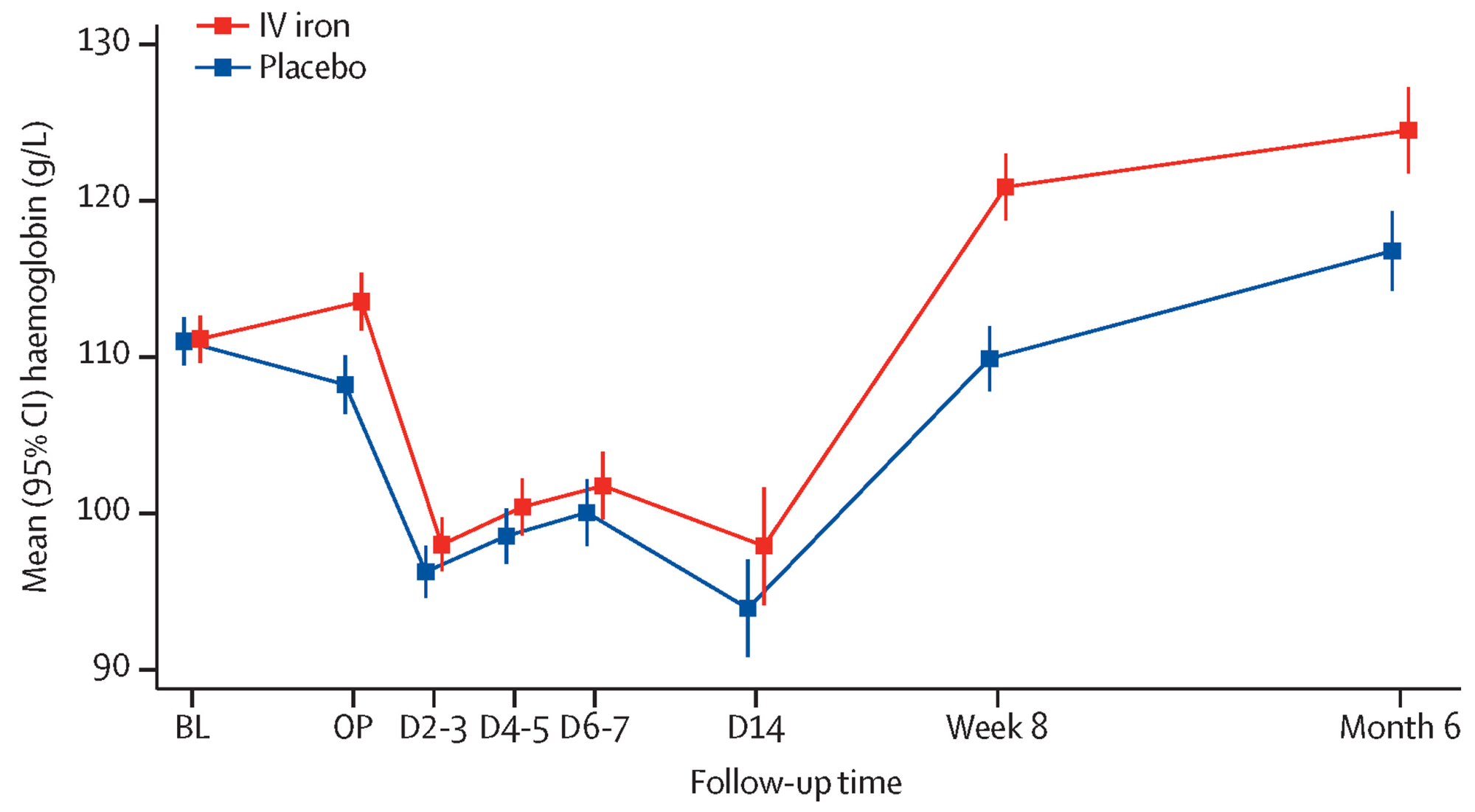
- Preoperative intravenous iron to treat anaemia before major abdominal surgery - PREVENTT - Lancet 2020
- The PREVENNT randomised, double-blind, controlled trial of preoperative intravenous iron to treat anaemia before major abdominal surgery - an independent discussion - BJA 2021
- The Association Between Iron Deficiency and Outcomes - a Secondary Analysis of the Intravenous iron Therapy to Treat Iron Deficient Anaemia in Patients Undergoing Major Abdominal Surgery - 2023
- Recommendations From the International Consensus Conference on Anemia Management in Surgical Patients (ICCAMS) - 2023
- The Important Role for Intravenous Iron in Perioperative Patient Blood Management in Major Abdominal Surgery - Annals of Surgery 2016